
Level One Trauma Center Prioritizes Equitable Healthcare Delivery During COVID-19
When the global coronavirus pandemic struck in 2020, Hennepin Healthcare wanted to make sure its most vulnerable patient population would receive equitable healthcare services. This level-one trauma center based in Minneapolis, Minnesota, looked closely at things like Medicare and Medicaid reimbursements as they pertained to telehealth services as well as the technology required to deliver virtual care during the pandemic.
“Like many healthcare facilities, we were thrust into telemedicine during the pandemic,” said Dr. Ryan Jelinek, clinical informatics fellow at Hennepin Healthcare. “We built solutions with patient equity in mind and have a committee that keeps an eye on that equity as we add services. Our community needs assessment showed us that 89% of our patient population actually had the technology required for telehealth but often didn’t know how to use it.”

Photo description: Hennepin Healthcare
Creating More Equitable Technology Platforms
The first issue that Hennepin Healthcare tackled was how to ensure that telehealth video visits could be conducted in a manner that was equitable for those patients who did not speak English or were not well-versed in how technology worked.
“Our main way of connecting with patients in the beginning was an integrated video visit using Zoom embedded in our electronic health record (EHR),” Jelinek said. “It was inherently inequitable because it was only available in English and demanded a certain level of tech literacy.”
Hennepin Healthcare developed a custom pathway that allowed patients to connect through a simple SMS text link provided by a third party. In addition, a reminder service translated the text communication into Spanish and Somali, which facilitated much better communications between provider and patient.
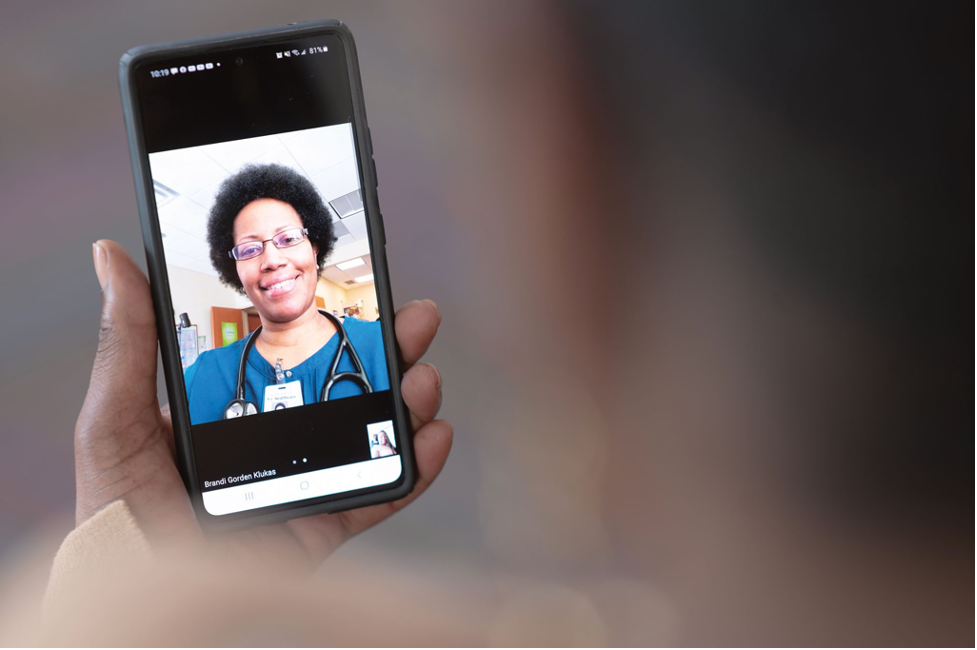
Photo description: Hennepin Healthcare provider conducting a video visit
Looking Closely at Language
A second component of working to improve communication between Hennepin Healthcare and its more vulnerable patient population looked at translations of common telehealth terminology and literacy levels.
“We reviewed our recordings of patient-provider interactions and quickly learned that words and phrases such as ‘in-person’ and ‘virtual’ don’t translate well into Spanish and Somali,” Jelinek explained. “We then worked to change how we were describing our services and the interactions required and brought language to a fourth-grade literacy level.”
In addition, Hennepin Healthcare developed patient-focused toolkits to help them succeed in the new world of telemedicine. “Our PDF and video-based tools were very visual, at a fourth-grade literacy level and translated into Spanish and Somali,” Jelinek said. “Patients were encouraged to review their toolkit 48 hours before their telehealth visit. The toolkit helped explain how to connect for their visit and how to access information. It also reminded them to find a private, quiet spot and a way to keep their phone still during the visit by doing something as simple as placing it inside a bowl.”
Jelinek said that patients seem to appreciate this modality of healthcare, and that their efforts in providing equitable care to different minority groups seems successful. “Back in March, less than 2% of our telemedicine visits were completed by non-English speaking patients. By November this had grown to over 12%.”

Photo description: Hennepin Healthcare scribe
Training Residents Key to Future Expansion of Telehealth
Besides ensuring that Hennepin Healthcare’s most vulnerable patients had equitable access to healthcare, Jelinek has also been working closely with training resident doctors in the virtual technology.
“Many of our residents don’t initially see how telehealth can deliver an adequate level of care,” Jelinek said. “I remember a situation when I was working with a resident. Our patient had multiple substance use disorder and mental health issues and had become agoraphobic during the pandemic. We managed to set up a telehealth appointment and started chipping away at the chronic healthcare issues as well as providing some financial counseling and medication refill check-ins.
“After the first appointment, the resident thought the patient would never show up for the second appointment, and I said she didn’t need to show up, she just needed to answer her phone,” he continued. “After three telehealth appointments, she was in a much better place. Instead of hospitalization, which was a very real possibility, we had her medications refilled and she was stable.”
As telehealth technology continues to grow, finding unique and effective ways to treat patients in their homes hold many potential opportunities. “There is a power to this type of healthcare that we don’t have in a sterile office environment,” Jelinek reflects. “We can be virtually present in patients’ homes and see what their social drivers or determinants of health actually look like. We can see them in action, peek into their living environment. We can see what’s in the fridge and medicine cabinet.”
Jelinek noted that patients also seem to be more comfortable conversing from their homes, and that leads to a fruitful conversation that can uncover other healthcare concerns that can then be addressed more successfully.

Photo description: Hennepin Healthcare lobby
